



Theme
Student as teacher
INSTITUTION
HeatlhPEER (Health Professions Education and Educational Research)
Monash University
Peer Assisted Learning (PAL) may be useful in building graduates’ life-long ‘non-technical skills’, such as communication, teamwork, time-management and self-direction (1).PAL also confers benefits in its potential time efficiency for both staff and students as compared to traditional placement structures (2). Studies of PAL in clinical placements have largely focussed on assessment (3,4). Little is known about formal (structured) or informal PAL in medical students’ clinical placements.
Monash University runs a hybrid PBL-lecture, five-year undergraduate and four year graduate entry medical program in Australia. PAL activities are incorporated into the pre-clinical years; there are fewer formal PAL structures on clinical placements. In 2012, students in their first clinical year were asked to complete an online survey, which collected information on their PAL usage, and perceptions of PAL utility, advantages and disadvantages.
54 students responded from metropolitan, rural and international (Malaysia) sites. The most useful activity for students’ learning needs was being taught by a peer, and the least useful was giving feedback to a peer (Table 1). The most frequent activity reported was discussing a case with a peer; the least was having a skill demonstrated.
| How useful was this activity for your learning needs? * | Male % | Female % | Total % |
Average weekly frequency |
| I was taught by a peer about a topic | 89 | 86 | 87 | 2.96 |
| I taught a peer about a topic | 83 | 85 | 86 | 2.24 |
| I was observed by a peer performing a history/examination | 71 | 93 | 85 | 2.43 |
| I received feedback from a peer on my performance/knowledge | 69 | 88 | 81 | 1.83 |
| I discussed a case wtih a peer | 82 | 74 | 77 | 3.65 |
| A peer discussed a case with me | 75 | 74 | 74 | 3.37 |
| A peer demonstrated a skill to me | 64 | 77 | 72 | 1.11 |
| I observed a peer performing a history/examination | 53 | 80 | 70 | 3.31 |
| I demonstrated a skill to a peer | 57 | 76 | 69 | 1.26 |
| I gave feedback to a peer on their performance/knowledge | 53 | 59 | 57 | 2.15 |
| TOTAL | 70 | 79 | 87 | 24.31 |
*Responses were measured on a scale of 1 = not at all useful to 5 = extremely useful, with no intermediary descriptors used for points 2, 3 and 4. In the above table, responses greater than 3 were pooled.
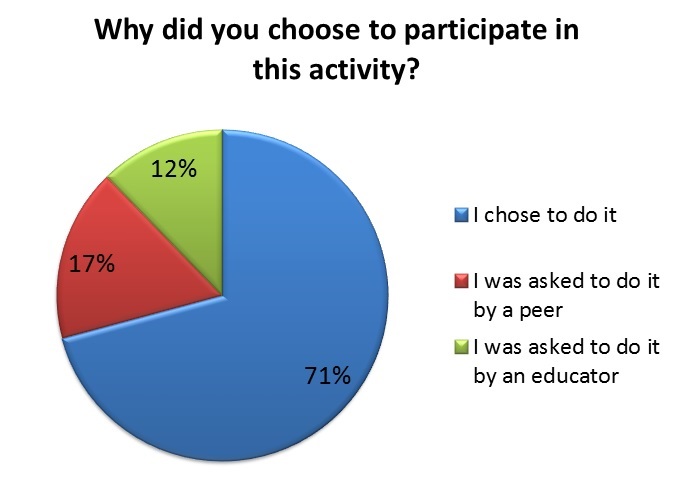
Figure 1. Reasons for participation in PAL activities
PAL was largely self-initiated as opposed to educator prompted or peer prompted (Figure 1). A proportion was undertaken in informal settings such as the student common room, outside the hospital, in the cafeteria and on the wards (Figure 2).
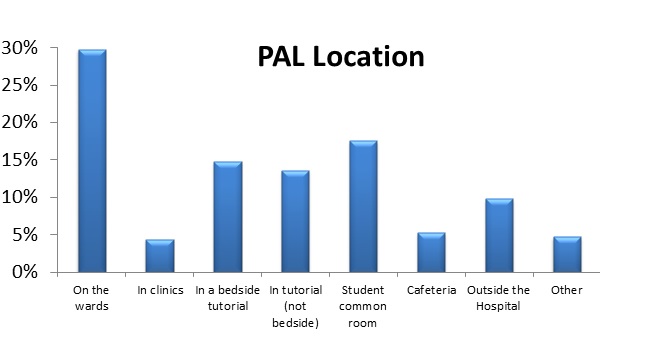
Figure 2. Locations of PAL activities
There was high agreement that PAL allowed students to measure their progress against peers (78%), improved teaching skills (74%) and increased understanding (72%). Forty-one percent of students felt uncomfortable giving their peers feedback, and 41% reported that they did not trust their own judgement on their peers’ knowledge or performance.
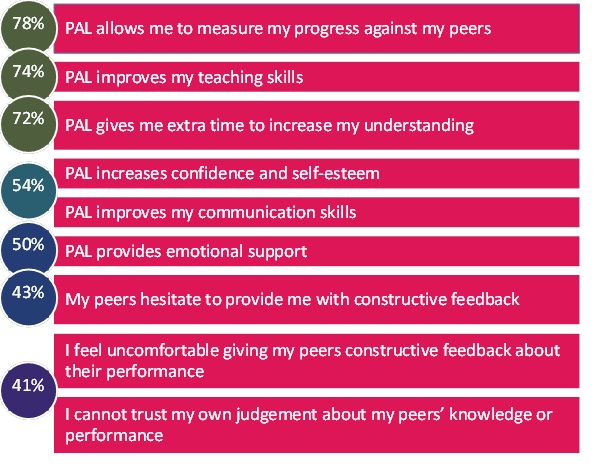
Figure 3. Percentage of students who agreed or strongly agreed with PAL statements
PAL may contribute not only to content learning, but also the development of non-technical skills such as self-directed learning and teamwork. This study demonstrated that a proportion of PAL on clinical placements occurs in informal, non-structured settings. Exposure to formalised, facilitated PAL in pre-clinical years may orientate learners to PAL’s purpose and benefits. Further investigation of how PAL is enacted in the clinical environment is required.
- Students voluntarily use PAL on clinical placements: this occurs mainly in informal settings
- Students report feeling challenged by making judgements about the quality of a peer's performance and communicating this in the form of verbal feedback
-
PAL benefits could be enhanced through:
- orienting learners to PAL methods and outcomes
- providing learners and educators with frameworks for supporting PAL
- Lincoln MA, McAllister L. Peer learning in clinical education. Medical Teacher. 1993;15(I):17–25.
- Ladyshewsky RK. Enhancing service productivity in acute care inpatient settings using a collaborative clinical education model. Physical therapy. 1995 Jun;75(6):503–10.
- Levine R, Kelly P, Karakoc T. Peer evaluation in a clinical clerkship: Students’ attitudes, experiences, and correlations with traditional assessments. Academic Psychiatry. 2007;31(1):19–24.
- Kovach R a, Resch DS, Verhulst SJ. Peer assessment of professionalism: a five-year experience in medical clerkship. Journal of general internal medicine. 2009 Jun;24(6):742–6.
 Send Email
Send Email