
 |
Title
Does simulation training help to prepare final year medical students for their roles as junior doctors?
Theme
10BB Simulation 2

Background
In recent years the use of simulation as a teaching tool has risen in popularity. Advances in educational technology have had an important impact with the General medical Council (GMC) advising that medical schools take advantage of new technologies, including simulation, to deliver teaching.1
But is it useful in preparing medical students for their roles as practitioners and does it add anything not provided by traditional teaching methods?
Summary of Work
At Pinderfields Hospital we have introduced a simulation course for our 5th year medical students. Within the first year of introduction 133 students attended the one day teaching session. Students had the opportunity to both participate and observe the management of the acutely unwell 'patient' in a simulated ward environment.

Summary of Results
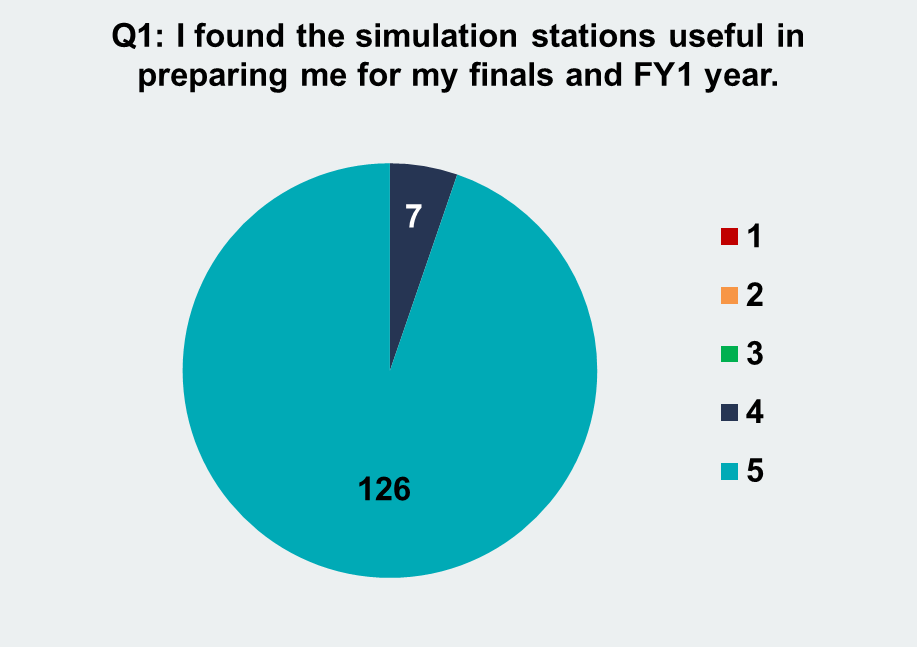
After each session we provided the students with a feedback form. Each question was scored between 1 and 5, with 1 meaning that the student strongly disagreed with the statement and 5 meaning that the student strongly agreed. There was also the opportunity to give free text feedback. When asked to score the statement "I found the simulation stations useful in preparing me for my finals and FY1 year": 95% of students strongly agreed.
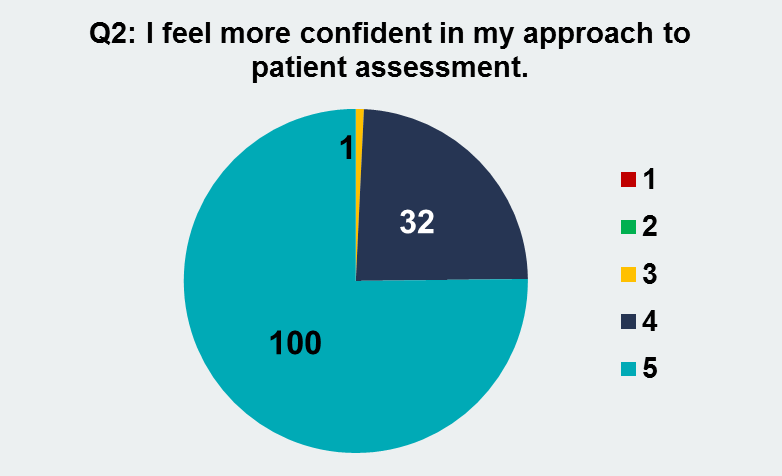
When asked to score the statement "I feel more confident in my approach to patient assessment": 75% of students strongly agreed and 24% agreed.
Conclusion
At an undergraduate level, simulation teaching allows medical students to experience the stress and responsibility of caring for acutely unwell patients without compromising patient safety.2 This is especially useful for final year students preparing to start their work as doctors.3 Introducing stress does not appear to have a negative impact on learning.4
Our sessions agreed with these findings. The students found our sessions to be a stimulating representation of real-life situations. They felt challenged and yet safe.
"BRILLIANT. It was really nice to be in an almost real life situation with the stress and sweat actually happening. The simulators were excellent, really wish they were available everywhere for training"
"An excellent opportunity to practice scenarios. Has made me much more confident in my abilities to recognise and treat patients with acute problems"
Debriefing addressed clinical themes and allowed us to expand on human factor issues that may not have been addressed in such depth previously. Feedback is thought to be key in ensuring effective learning in simulation based teaching.5
The students found this method of teaching extremely useful. They felt that it had helped to prepare them for their roles as new doctors in a way that had not been possible with the more traditional teaching methods.
Take-home Messages
Simulation is a successful and valid tool for preparing medical students to become practitioners. It is a useful addition to more traditional teaching methods.
Acknowledgement
Thank you to the simulation team (Zakir Chopdat, Fiona Coia, Reshad Khodabocus, Kevin Ross and Adam Smith) at Pinderfields Hospital who have helped to make this such a popular, fun and successful teaching venture.

References
1. Tomorrow's Doctors: Outcomes and Standards for undergraduate Medical Education. GMC September 2009.
2. Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N, Morrison J, Donaldson M, Whitelaw M, Field M. How prepared are medical graduates to begin practice? A comparison of three diverse medical schools. London: General Medical Council Education Committee; 2008.
3. Tallentire VR, Smith SE, Skinner J, Cameron HS. Understanding the behaviour of newly qualified doctors in acute care contexts. Med Educ 2011; 45: 995-1005.
4. Macdougall L, Martin R, McCallum I, Grogan E. Simulation and stress: acceptable to students and not confidence-busting. The Clinical teacher 2013; 10: 38-41.
5. Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach 2005; 27: 10-18
