


Theme
3JJ Staff development
INSTITUTION
MGH Institute of Health Professions, Health Professions Education Program, Boston
Harvard Medical School
Massachusetts General Hospital

Introduction and Problem
Current state of faculty readiness for IPE:
- Assumed IPE teaching skills based on clinical experience
- Little or no preparation - trial and error or just in time training
- Pedagogy based - teaching practices intended for children
- siloed formal education degrees
- e.g. medical or nursing education
The problem:
- Most faculty are not ready for IPE-based education
- do not learn about IPE in interprofessional context
- Minimal literature defining effective faculty preparation for IPE
- Students are expected to learn together,
...yet faculty preparation remains siloed
MGH Institute as IP Context
A graduate school founded by Massachusetts General Hospital,
- Broad portfolio of non-medical schools
- PA, nursing, PT/OT, SLP
- >1,200 student population
- Graduate school: admit only post-baccalaureate applicants
- Interprofessional Dedicated Educational Unit (iDEU) at MGH
- Crimson Care Collaborative:
- With Harvard Medical School
- MD and NP student run clinic
Successful certificate program for educators across professions
|
Network of collaborators
|
|
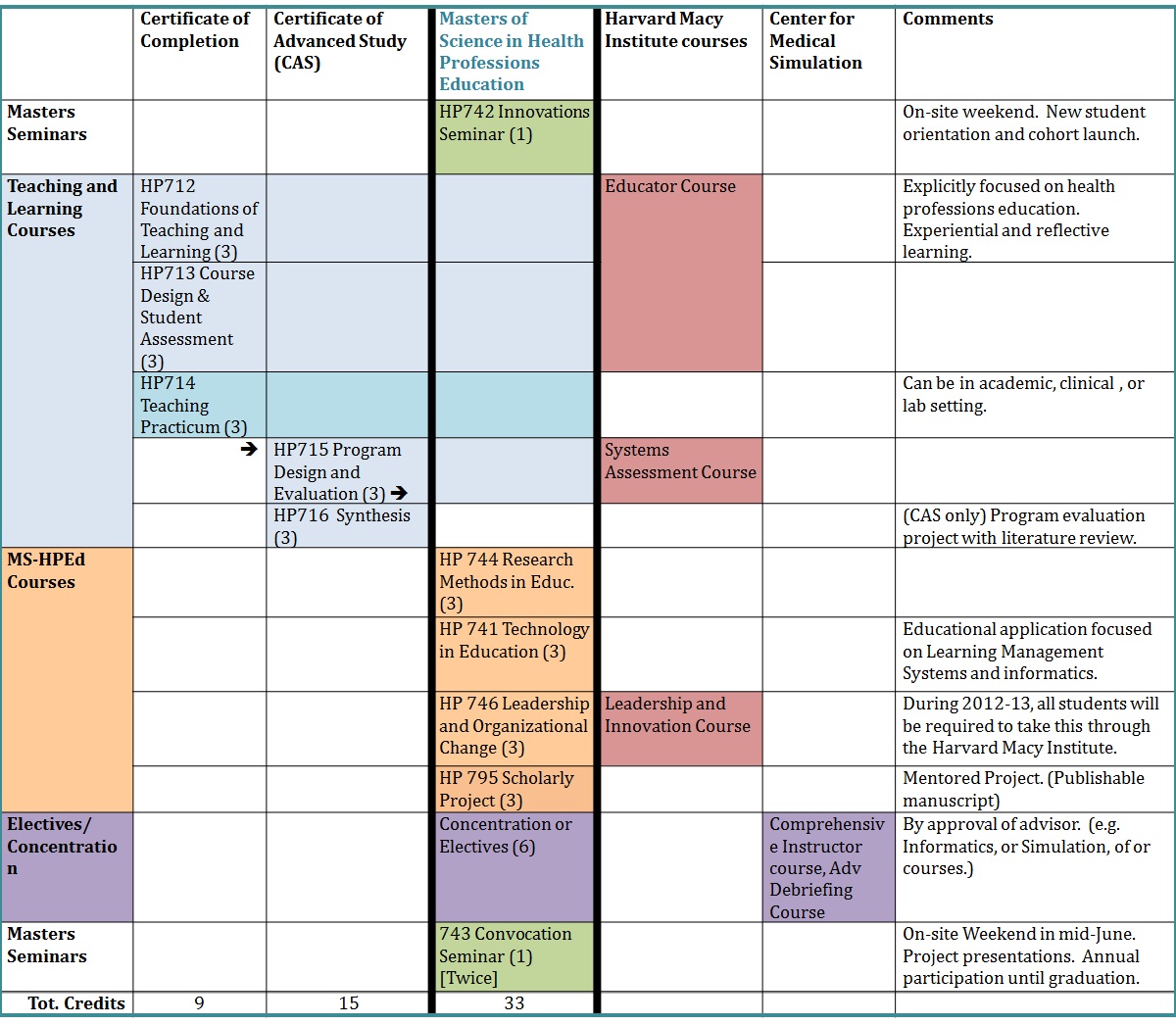
Masters Degree for IPE-ready Faulty Teams
- The Health Professional Education (HPEd) Program offers an explicitly interprofessional context for post-professional education
- Interprofessional Leadership:
- Nursing, medicine, and physical therapy
- Advanced degrees in education
- Blended Advisory Committee
- Interprofessional Leadership:
- Modeled after the executive MBA programs:
- On-site intensive sessions and online learning
- Accessible to working clinician/educators:
- Multiple points of access and pathways through collaorators
Methods and Data Souces
Program efficacy monitoring was put in place as the first cohorts were admitted.
Benchmark data collected. Sources of data include:
- Scholarly productivity: course projects, papers, publications
- Faculty evaluation of scholars and courses
- Stakeholder input from HPEd Advisory Committee
- Student survey at course, program, and professional levels
- Professional impact survey cv review of students and alumni
Survey Results and Discussion
Survey sample:
- 23 alumni and 25 current scholars
- Representing medicine, pharmacy, clinical psychology, PT, and ed admin.
- From 6 US states and six countries
- Mean age 47 years
- Years of clinical practice (mean) – 12.3 years
- Years in academia (mean) – 11.5 years
- ~ 90% finished in two years part time study
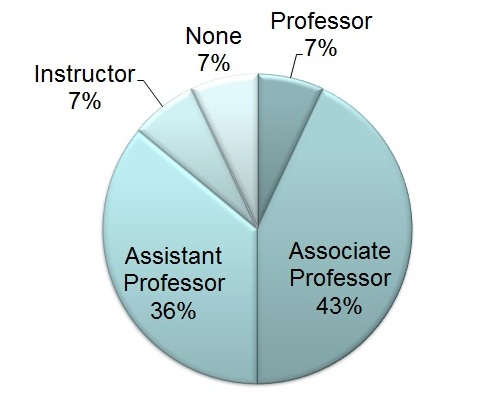
Academic rank in 2013
- 50% assoc. or full professor
- 36% asst. professor
Stated reasons for choosing this MS-HPEd program
- 73% rated IP nature of program as
- influencing their choice of program positively
- 91% chose this program because of access through collaborators
As a result of this MS-HPEd program:
- 56% listed IP related topics as their greatest take-aways from the program.
- “[I learned to] create educational opportunities for broader groups.”
- “I am now part of an educator community … across professions.”
- “[I am] more confident reaching out [to other] professions for projects.”
- “I can now train a new generation of educators with broad impact”
- 67% will be taking on additional administrative responsibilities
- 100% strongly agreed that “this program increased my understanding od educational challenges facing other professions.”
- 100% agreed that they “improved my IP relationships at my [work place]”
Conclusion:
Un-silo-ing graduate programs for educators may be the next challenge across health professions to create truly unified IPE-ready faculty teams.
Future impact studies will include:
- Interprofessional attitudes survey
- IP projects started and completed
- Publications with IP co-authorship,
- Publication in education journals,
- Promotions, and new roles of educational leadership
Tekian, A (2012) Preparing health professions leaders worldwide: A description of masters-level
education, Medical Teacher. 34 (1).: 52-8.
Bearman, M, Dawson, P (2013) Qualitative Synthesis and Systematic review in health professions
education. Medical Education. 47 (3): 252-60

.jpg)

 Send Email
Send Email