


Theme
Postgraduate Education
INSTITUTION
Royal College of Surgeons in Ireland
Beaumont Hospital, Dublin

1-2% of patients sustain harm as a result of medication errors, the majority of which are related to prescribing.
Whilst all prescribers make mistakes, junior doctors are most prone to prescribing errors. In addition, errors are often grossly under-reported by junior doctors.
Increasing junior doctors’ knowledge may reduce prescribing error and increase error reporting. Our study is evaluating the effect of a multi-faceted programme of education on junior doctors' prescribing and error reporting, in one national tertiary referral centre.
A clinical audit of prescribing errors, made by junior doctors whilst prescribing cardiovascular, anti-microbial, anti-psychotic, analgesic, anti-coagulant and hypoglycaemic agents was carried out on seven wards. Identified reportable errors were cross-referenced with the Medication Safety Coordinator to determine reporting compliance.
Criteria and standards for audit were established by combining the best practice of several organisations with hospital policy and protocols. The completeness of documentation of patient and administrative details was also audited.
An education strategy was developed, based on the audit results, and delivered to junior doctors by a Clinical Lecturer. It encompassed both verbal and written feedback of the audit data and information on good prescription writing practices, using worked examples. Online tutorials, facilitated remediation and supervised prescribing are to be incorporated into the programme at a later date.
A re-audit was peformed to assess the impact of this education. Analysis of the re-audit results is on-going.
The prevalence of prescribing errors in hospital medication orders may be higher than that previously reported in the literature.
Junior doctors, specifically interns, are our most frequent prescribers, and make errors regularly when prescribing. Errors occur most commonly in the physical act of writing a medication order.
Junior doctors appear disengaged with the error reporting process, and are non-adherent to error reporting protocols.
The preliminary programme of education delivered to junior doctors did not significantly improve their documentation of patient and administrative details on drug charts.
Identifying the authors of erroneous medication orders remains a challenge, due to the inconsistent documentation of prescriber pager numbers on medication orders.
Prescribing errors are a significant cause of morbidity and mortality for patients.
Education and feedback can be effective in reducing prescribing errors and increasing error reporting amongst junior doctors. Educators and clinicians should therefore endeavour to provide regular and meaningful feedback to prescribers.
Changing prescribers’ behaviours through education and feedback is most effective when it focuses on areas where there is strong evidence linking processes and patient outcomes.
This group will continue our efforts to create a comprehensive and pro-active programme of feedback and education for prescribers, with the ultimate aim of reducing prescribing errors and increasing error reporting.
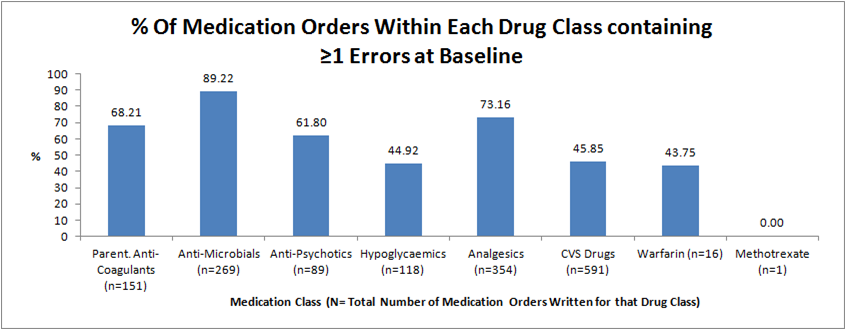
Figure 1 - Percentage of medication orders containing one or more prescribing errors in each drug class at baseline.
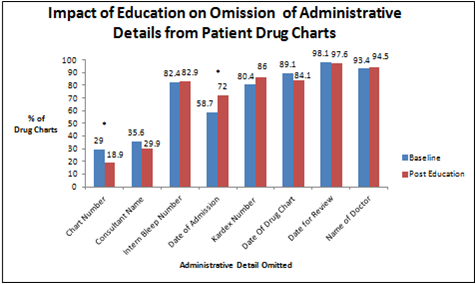
Figure 2 - Impact of education on the omission of administrative details from patient drug charts. * indicates p<0.05 as determined by the student's t-test.
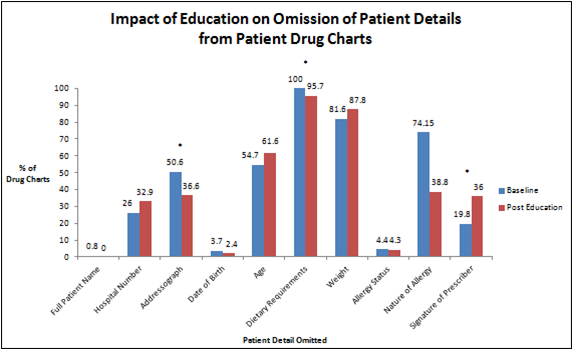
Figure 3 - Impact of education on omission of patient details from patient drug charts. * indicates p<0.05 as determined by the student's t-test.
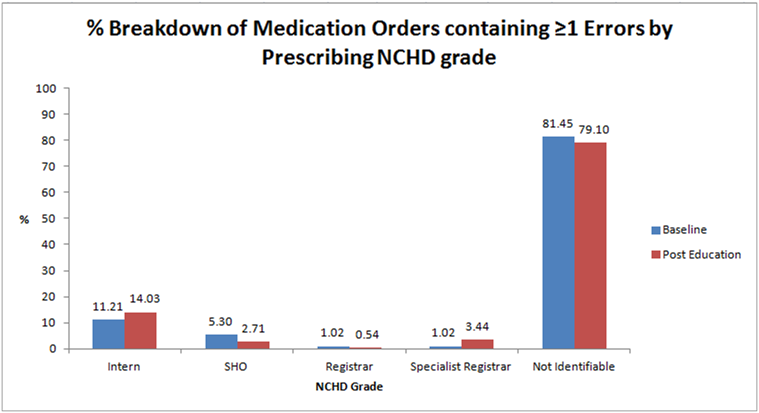
Figure 4 - Percentage breakdown of medication orders containing one or more errors by prescribing non-consultant hospital doctor (NCHD) grade. SHO = Senior House Officer.
 Send Email
Send Email