


Theme
9AA Teaching and assessing communication skills
INSTITUTION
Perelman School of Medicine at the University of Pennsylvania - Philadelphia - USA
Group Health Cooperative and University of Washington - Seattle, USA
University of North Carolina, Chapel Hill, USA, AXDEV Group, Brossard, Canada

Effective self-management behaviors by patients with T2D can reduce co-morbidities, mortality risk, and overall healthcare costs. Challenges in inter-professional (IP) communication in primary care teams (PCTs) and effective patient-provider communication contribute to patients’ disengagement, non-adherence and undermine HCP’s confidence and professional fulfillment.
Can Provider Communication Impact Patient Adherence?
Effective provider-patient communication is linked to improved patient satisfaction, health status, recall of information, and adherence1-4
– Poor communication results in 19% higher risk of non-adherence
– Good communication results in 2.16-fold greater patient adherence
– Communication training results in 1.62-fold greater patient adherence

Our strategy was to provide evidence about importance of communication on T2D patients’ outcomes and to empower PCTs to practice effective communication skills within the context of the disease management.
The intervention was a half-day workshop including expert-led lectures, small group break-outs with standardized patients, interactive discussions and take away tools delivered 10 times across the US.
Intervention Design: Improving Adherence in T2D with Training in Communication “Talking Diabetes with Your Patients” worksho
- The Evidence and Building Knowledge Base (45 minutes)
- Adherence Challenges in T2D & Impact of Communication on Adherence
- New Concepts in Communication strategies
- Expert-facilitated rotating small group breakouts with Standardized Patients (SPs) (160 minutes)
- Peer-group Hands-on Practice with four unique cases to build competencies
- Included pee, expert and patient feedback (SP)
- Reinforcing Key Strategies: Putting it All Together –(60 minutes)
- Faculty and Participants Discussion:
- Resources, Tools, and Take-Away Pearls (giveaway practice algorithm and communication tool box)
- Hall JA, Roter, DL, et al. Meta-analysis of Correlates of Provider Behavior in Medical Encounters. Medical Care. 1988; 26(7):657-675.
- Stewart MA. Effective physician-patient communication and health outcomes: a review. Canadian MAJ. 1995;152 (9):1423-1433.
- Ong LM, de Haes, JC et al. Doctor-patient communication: A review of the literature. Social Science & Medicine. April 1995;40:903-918.
- Haskard Zolnierek, Kelly B, et al. Physician Communication and Patient Adherence to Treatment: A Meta-Analysis. Medical Care. August 2009; 47(8):826-34.
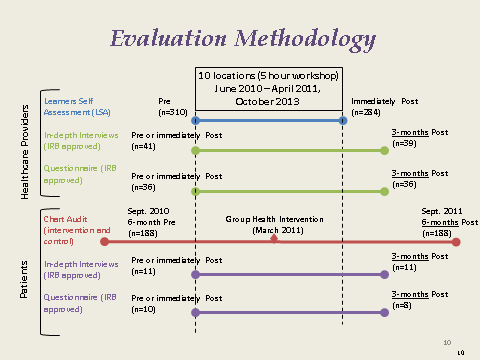
Mixed-methods, time-series, evaluation consisted of pre/post self-assessment questionnaires, evaluation questionnaires and 3 month post qualitative interviews, and pre/post 6 month patients’ chart audit with control.
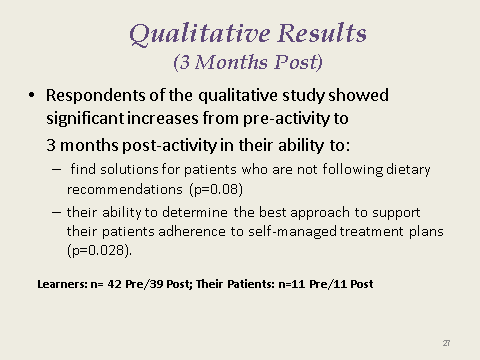
Increased knowledge of promoting positive self-management behaviors and confidence in ability to assess patients’ readiness to adopt treatment plans were observed (both p≤0.001). PCPs’ understanding of the impact of their communication approach on positive self-management behaviors and their role in facilitating adherence both increased significantly (p≤0.001).
Patient chart audits revealed significant increase in a number of health management indicators. Patients reported changes in PCPs attitudes and functioning of the PCTs.
Findings provide evidence of positive impact of IP, simulation-based interventions empowering PCPs to better communicate as a team and with their patients on clinical efficiencies and quality of care.
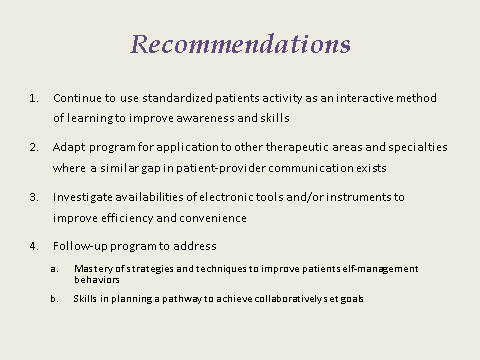
To ensure sustainable practice changes, it would have been beneficial to conduct additional reinforcing activities post-intervention.
Skills and strategies learned can be effective in other disease management settings.
This project was led by the Continuing Medical Education Program of the Perelman School of Medicine at the University of Pennsylvania and funded by educational grants from Sanofi-Aventis and Pfizer.
 Send Email
Send Email