


Theme
5BB Team Based Learning/Learning anatomy
INSTITUTION
Medical Education Center Phayao Hospital - Phayao - Thailand
Clinical teaching should ideally improve a medical students knowledge and change their behavior in daily practice towards a best clinical practice. There is good evidence to suggest that interactive methods such as team-based learning (TBL) can encourage sustainable knowledge and performance change as well as lead to high satisfaction among participants.
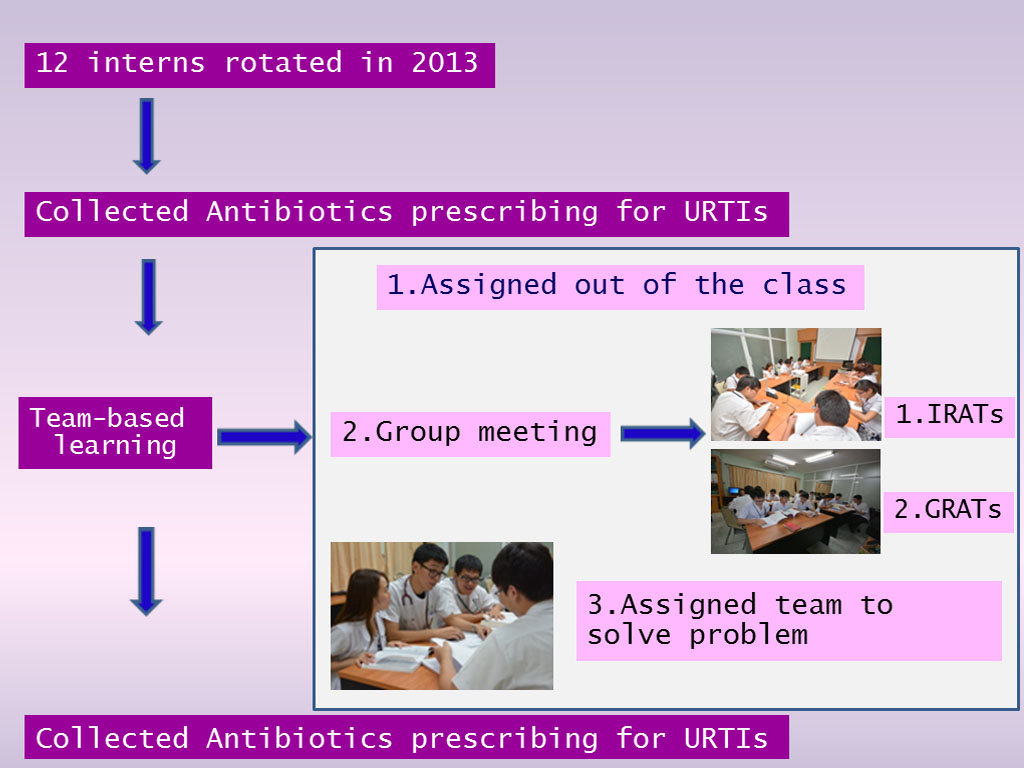
TBL was proven to promote active learning within a group of students for three reasons. First of all, group work is central to exposing students to and improving their ability to apply course content. Secondly, the greater part of class time is used for this group work. Lastly, TBL involves multiple group tasks that are designed to improve learning and promote the development of self-managed learning groups. However, there are fewer reports of its use in postgraduate medical education.
We designed an interactive seminar on "Antibiotics Smart Use" by using a team-based learning approach to evaluate whether it leads to improved behavior change in antibiotics prescribing for URTIs among Interns.
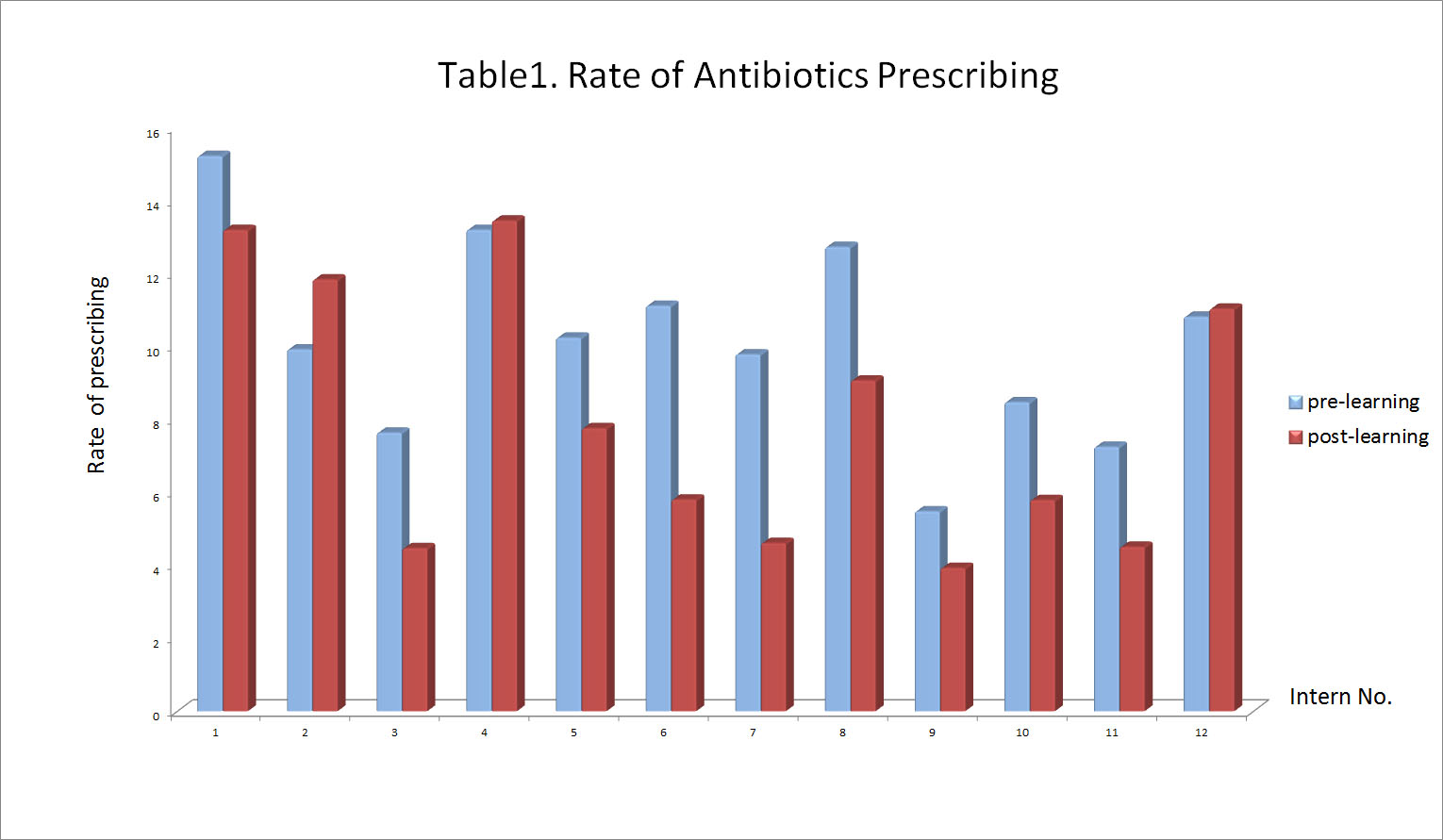
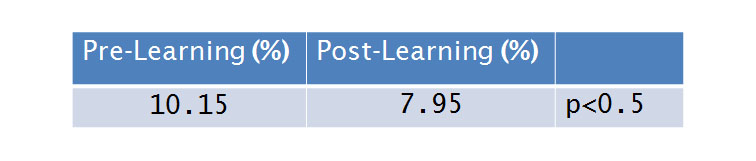
Table.2 Mean scores of anibiotic prescribing rate for URTIs
I wiould like to thank all interns who participated in the study, data collector and the director of Phayao Hospital, Phayao, Thailand. Furthermore, I would like to express my profound gratitude to Dr. Pannathorn Chachvarat, Boromarajonani College of Nursing Phayao, who helped in the analysis of data.
TBL can lead to a significant change behavior toward appropriate for antibiotic prescribing for URTIs of interns.
TBL can be successfully introduced into postgraduate trainning program and will indirectly improve patient care.
1. Smits PB, Verbeek JH, de Buisonjé CD: Problem based learning in continuing medical education: A review of controlled evaluation studies. BMJ 2002, 324:153–156.
2. Kiessling A, Henriksson P: Efficacy of case method learning in general practice for secondary prevention in patients with coronary artery disease: Randomised controlled study. BMJ 2002, 325:877–880.
3. Kiessling A, Lewitt M, Henriksson P: Case-based training of evidence-based clinical practice in primary care and decreased mortality in patients with coronary heart disease. Ann Fam Med 2011, 9:211–218.
4. G Naghme, KD Saied, N Ali: Is a Team-based Learning Approach to Anatomy Teaching Superior to Didactic Lecturing? Sultan Qaboos University Med J 2014, 14:120-125.
 Send Email
Send Email