


Theme
3BB The lecture and the flipped classroom
INSTITUTION
Faculty of Medicine, University of Toronto - Canada
Mount Sinai Hospital, Toronto
Sunnybrook Health Sciences Centre, Toronto
In 2010 the Future of Medical Education in Canada (FMEC) report recommended increased exposure to the community. Expansion into the community created a barrier, in that all seminars for our Anesthesia Clerkship rotation were held centrally. To allow these students equal access, videoconferencing was initiated; however there were often technical problems. There was a need to develop a new platform to deliver the curriculum. The “flipped classroom” has been proposed as a model for delivering medical education, where the learning occurs at home (outside the classroom) and the application of knowledge occurs in the classroom. This was an ideal format to remedy our problem.
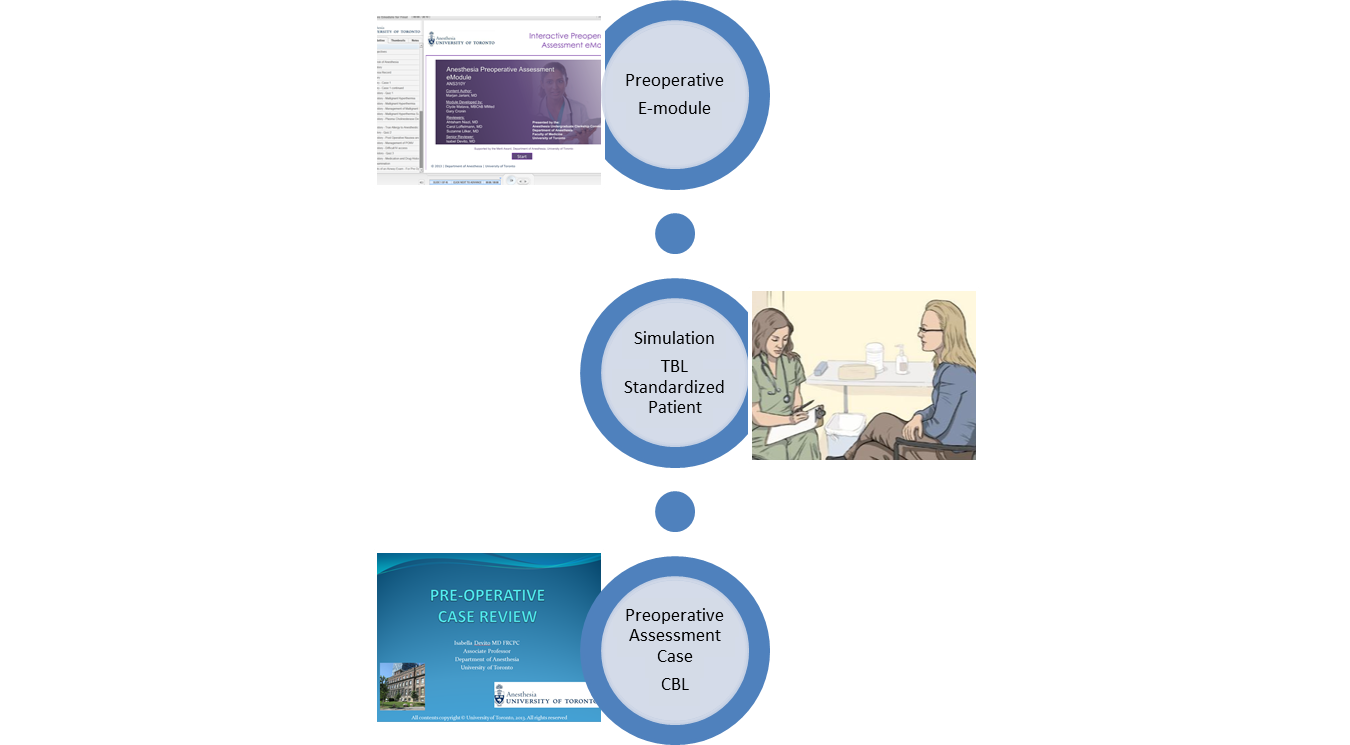
A flipped classroom was created where e-modules were used to replace the six core central seminars. Six interactive e-modules were developed, with pre and post module tests embedded within for self-assessment. Faculty were available through a discussion board to answer all e-module related questions.
Two of the six e-modules ( Introduction to Anesthesia and Team functioning & ACLS) were required to be completed prior to the introductory Simulation Day (Entry SimDay) held on the second day of the rotation. Content retention was reviewed at the start of entry simulation by use of multiple choice questions answered with i-clickers. Only content that was not globally answered well was reviewed prior to the start of the simulation day, which incorporated the knowledge learnt in the two e-modules.
In keeping with the principles of the flipped classroom, an Exit Simulation Day (Exit SimDay) was developed for the second last day of the rotation. Students working in teams (team based learning TBL) rotated through cases involving preoperative (with standardized patients), intraoperative and postoperative cases (using high fidelity simulation) and were scored as a team based on a checklist performance scale.
The Preoperative Case highlighted risk stratification, communication, preoperative assessment and management of the surgical patient. The Intraoperative case highlighted crisis management, mental practice, closed loop communication and team function in a high stakes environment. The Postoperative case highlighted situational awareness and acute pain management.
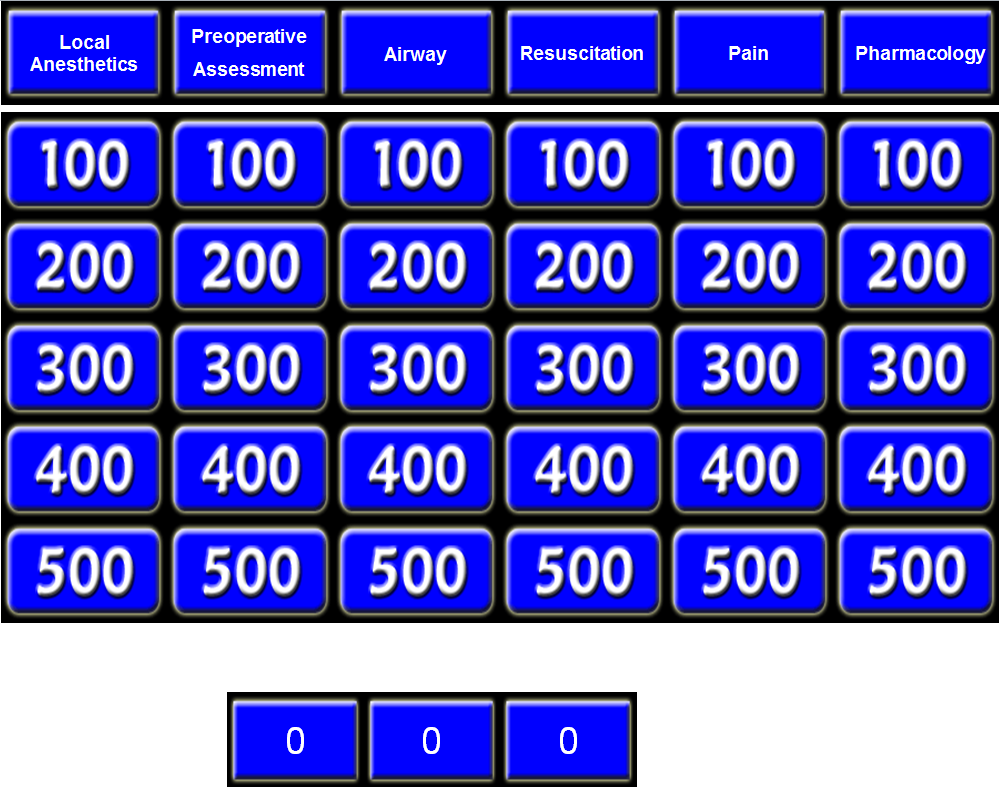
This was followed in the afternoon by case based learning (CBL) and a game of Anesthesia Jeopardy to review the e-module content and to allow them to integrate core knowledge.
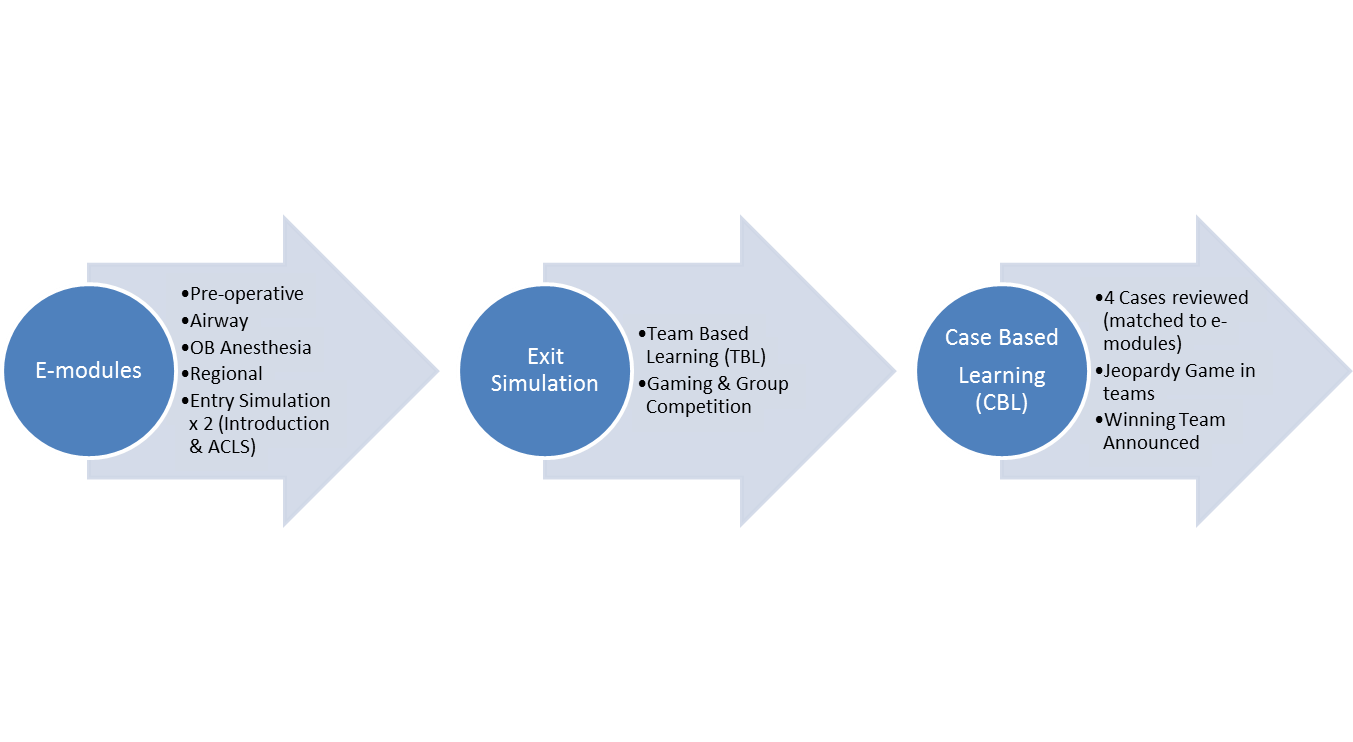
Four cases (CBL) were developed that mapped to the learning objectives of the other four e-modules. Gaming was a key component with team based scores (checklist score plus Jeopardy).
Anesthesia Jeopardy
The students compete in teams with subject matter highlighting core curriculum content.
We would like to thank all members of the Undergraduate Education Committee, Department of Anesthesia, University of Toronto for the collective vision and development of both the e-modules and the simulation days.
Five hundred students have rotated through the program to date. Results are positive, with common positive themes occurring in the evaluations. The e-modules have allowed for more clinical time and the exit simulation and CBL has allowed them to solidify and apply their knowledge.
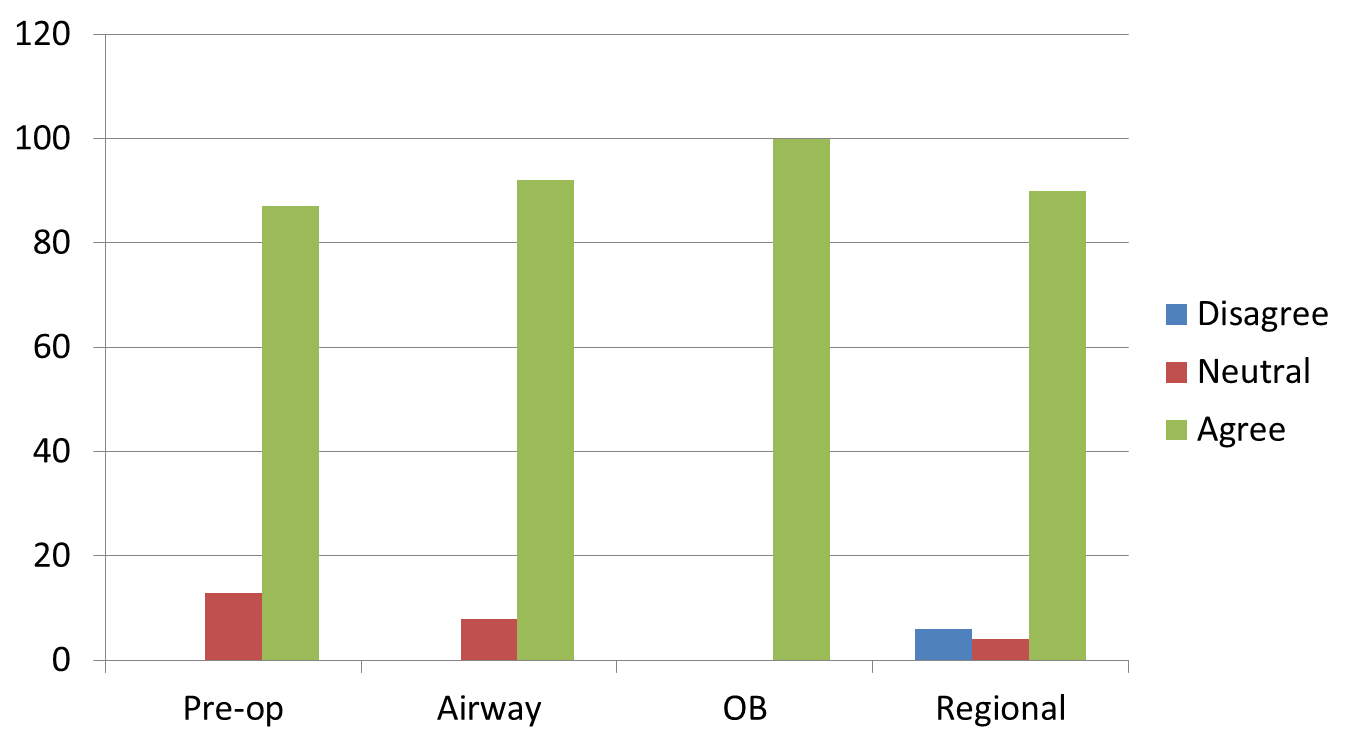
Evaluation Of Clerkship Components
(Seminars, E-modules, Simulation Days & Overall Rotation Evaluation- 5 Point Likert Scale, total responses)
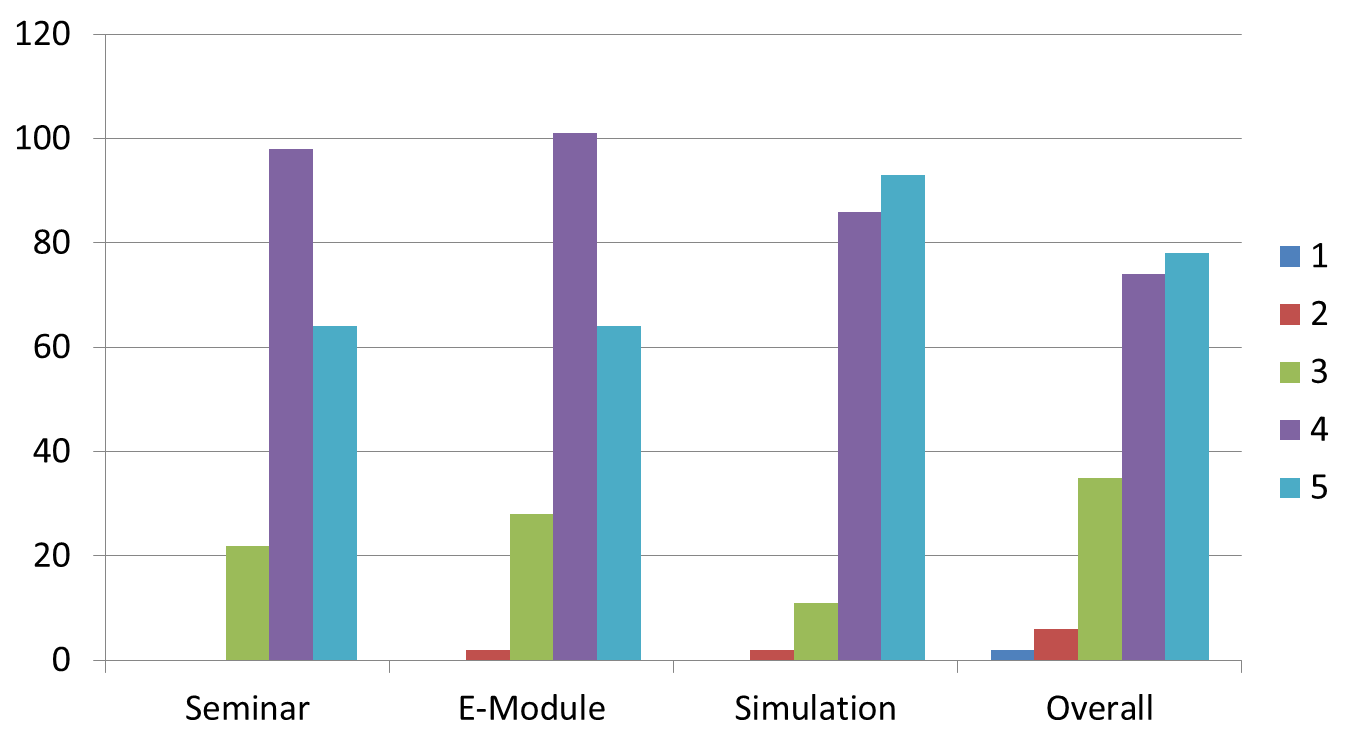
“Overall the Module was Excellent”
(As a Percentage of Students %)
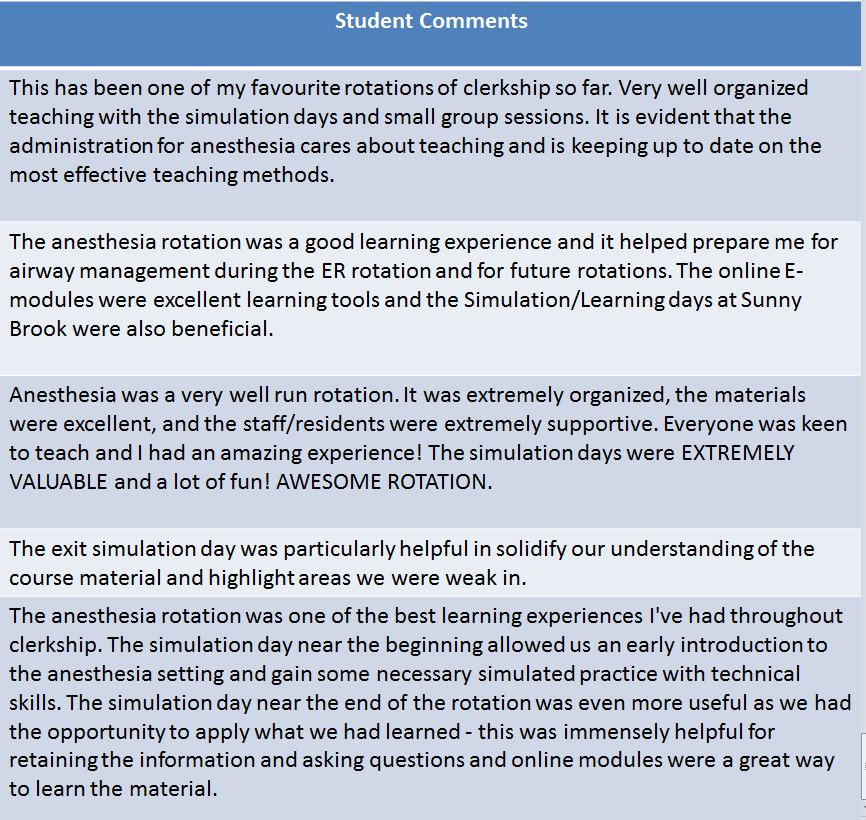
In alignment with the FMEC recommendations (community) and enabling recommendations (use of technology), a novel Anesthesia Clerkship Course was developed using the flipped classroom model. Results to date have been positive. Students are able to learn and review the e-module content outside of clinical time, allowing them more clinical exposure. They then attended an exit simulation where the knowledge learned through the modules was applied to clinical cases, thus allowing them to solidify and apply knowledge related to the core curriculum.
As we move forward to competency based medical education (CBME), this model of the flipped classroom may be useful for both undergraduate and postgraduate education.
- https://www.afmc.ca/future-of-medical-education-in-canada/medical-doctor-project/pdf/collective_vision.pdf (accessed August 2015)
- Prober CG, Heath C Lecture Halls without Lectures- A Proposal for Medical Education, N Engl J Med 366;18 1657-1659 May 2012
- 3. MClaughlin JE, Roth MT, et al The Flipped Classroom: A Course Redesign to Foster Learning and Engagement in a Health Professions School , Academic Medicine Vol 89 No 2 Feb 2014
 Send Email
Send Email