
| Theme: 10BB Simulation 2 | |||
 |
||||||
| Transposing problem based learning tutorials into high fidelity acute medical simulation: Familiarity promotes learning. |
 |
|||||
|
||||||
Simulated clinical scenarios are commonly used in undergraduate education. With unfamiliar scenarios, students generally demonstrate poorer performance in clinical and non-techincal aspects. This is compounded by the inexperience of students new to simulation. The stresses of unfamiliar clinical components in simulation are likely to impact negatively on effective learning of non-technical skills. By familiarising students with the clinical aspects of simulated scenarios, they will be able to concentrate on non-technical skills, responses and requirements of the simulation. This should promote learning and real-time reflection on the non-clinical challenges facing them.
This project aims to demonstrate that a familiar scenario with a predictable, pre-taught clinical course will provide a more efficient teaching platform for non-technical skills. An improvement in clinical confidence is also predicted by applying knowledge and skills acquired in a separate learning (small group tutorial) environment.
Groups of 8 students initially received tutorials on sepsis and haemorrhage, provided by a consultant anaesthetist. These sessions were developed by the University of Sheffield as specific problem based learning tools, known as “Integrated learning activities” (ILAs)1. Simulation scenarios modelled on each ILA were subsequently developed to instill familiarity, practice essential clinical skills and test non-technical skills. Metrics for non-technical skills were based on the Anaesthetist’s Non-technical Skills (ANTS) framework2. Students with no prior simulation experience completed scenarios in pairs, facilitated by a consultant anaesthetist, a number of trainees and clinical skills staff. These were carried out in a dedicated clinical skills facility with formal debriefing following each session. A pre and post scenario self-reporting questionnaire was utilised. These examined identical clinical and non-technical metrics, utilising an integer scale of 0-10. Data were collated and analysed using an excel spreadsheet.
Mean confidence levels for the identification and early treatment of septic patients increased from 4.1 to 6.7 and 3.5 to 6.8 respectively. Those for bleeding patients demonstrated a similar response, increasing from 4.5 to 6.7 and 3.2 to 6.6. A dramatic increase was demonstrated in the understanding of non-technical skills, improving from 1.8 to 7.3, with individual components (team working, task management, situational awareness and decision making) improving by 0.8, 1.4, 1.6 and 1.8 points respectively. Finally, the quality of the sessions was demonstrated by the scores of 9.0 for relevance to the stage of training, 9.5 for usefulness of the sessions and 9.6 for whether recommendations would be made to fellow students. 95% of students also found the simulation to be of an appropriate difficulty level.
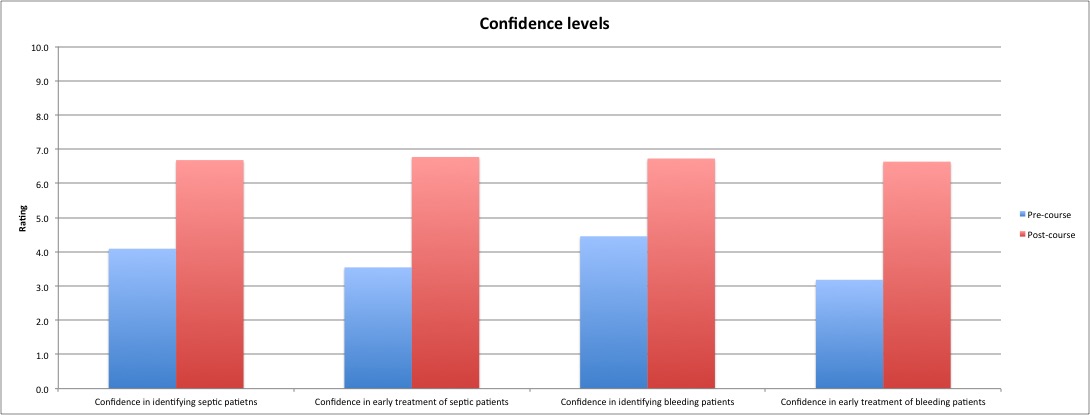
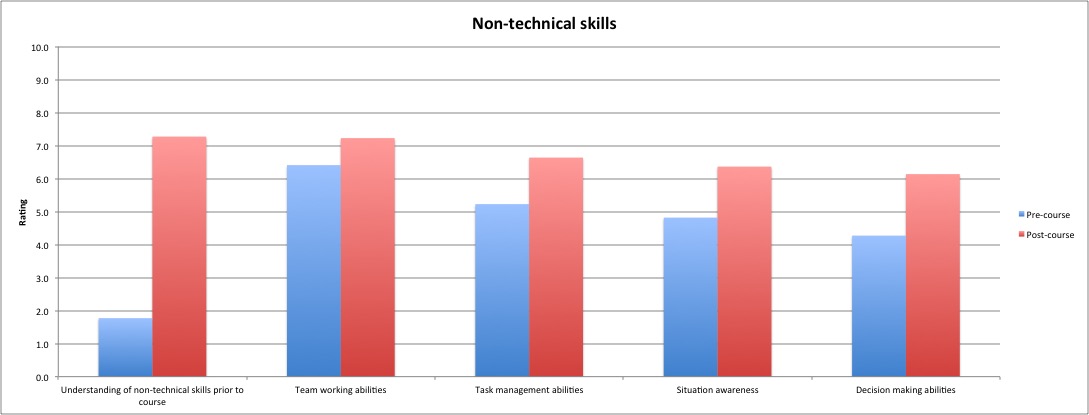
Figure 1. Self-reported student data
We demonstrated that clinical simulation mirroring pre-taught ILAs can provide an effective learning environment for non-techincal skills. An improvement of self-reported confidence in the recognition and management of acute clinical problems was also shown.
Non-technical skills within an acute clinical environment are difficult to teach and to learn. By simulating this environment and reducing the stress of clinical decision making through pre-taught ILAs, it is possible to bring focus on learning and reflecting on the non-technical aspects built into each scenario. This project provides a promising model for delivering a package of education specifically providing focus on non-technical and clinical skills for medical students.
1.https://www.shef.ac.uk/medicine/prospective_ug/mbchb (Accessed 8/8/15)
2. http://www.abdn.ac.uk/iprc/ants/ (Accessed 25/1/15)

 Send Email
Send Email