


Theme
8JJ Patient safety
INSTITUTION
St George's Hospital
1. Anaesthetic Trainee
2. Consultant Anaesthetist

In 2009 the WHO surgical safety checklist was introduced1. This is now standard practice with evidence showing it improves team communication and patient outcomes2.
In 2011, the Royal College of Anaesthetists and the Difficult Airway Society produced the 4th Royal College of Anaesthetists National Audit Project (NAP 4)3, looking at major complications of airway management in the United Kingdom. This demonstrated that at least one in four major airway events reported was from the Intensive Care Unit (ICU) or the emergency department(ED). Furthermore, the outcome of these events was more likely to lead to permanent harm or death than the same event occurring in the theatre environment.
One of the recommendations of the audit was that checklists and debriefing should be introduced into the emergency situation.
We had previously carried out a retrospective audit of 65 patients who required intubation, outside of theatres. We looked at documentation and the use of checklists. We concluded that documentation was poor and there was no evidence of checklists or debriefs being used.
After this audit, a checklist was introduced to aid the multi‐disciplinary team performing rapid sequence intubation (RSI) in the emergency department (ED). We then designed a survey to monitor staff members ’attitudes toward the checklist. The aim of this project was to identify and understand barriers to the implementation of visual aids.
Our survey demonstrated cognitive dissonance on the part of our anaesthetists. Whilst as a group they subscribed to use of the WHO checklist, they did not translate the learning from this to other situations.
There is need for ongoing promotion and training in the use of the checklist. We demonstrated barriers to the introduction of a checklist and have identified ways to improve this. In general, attitudes towards the use of a checklist are positive. In the future, training will be carried out using the checklist to improve mental modelling and team cohesion.
Multi-disciplinary team training is now being carried out using the checklist and shadow board to try and improve mental modelling and team cohesion.
1. A surgical safety checklist to reduce morbidity and mortality in a global population. Hayes et al. NEJM. 2009 306 491-499.
2.Do checklists improve teamwork and communication in the OR? A systematic review. Russ et al. Ann Surg. Dec 258(6)856-71.
3. www.rcoa.ac.uk/system/files/CSQ-NAP4-Full.pdf
We sent electronic and paper copys of our survey to all consultant and trainee anaesthetists, emergency medicine (EM) doctors and ODP's. We had 52 responses (5 ODP's, 1 EM doctors and 46 anaesthetists).
71% were aware of the new checklist and 42% used it routinely in the ED.
85% of respondents like the concept of a checklist.
20% of people had seen the checklist prevent a near miss.
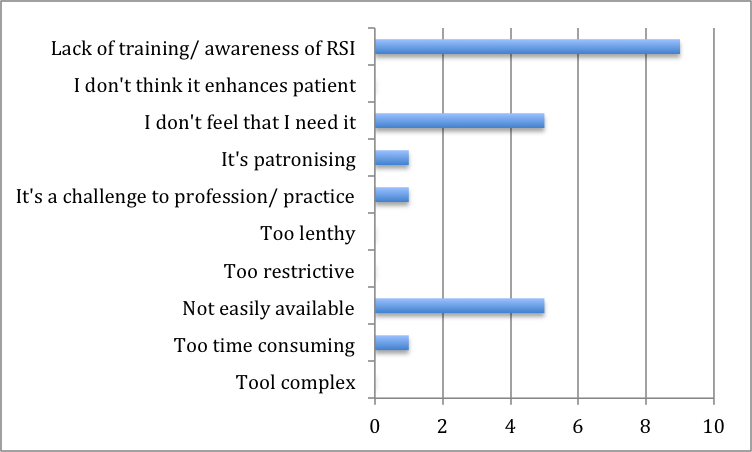
We asked: if you don't use the checklist routinely, why not?
We asked: What would improve your use of the checklist?

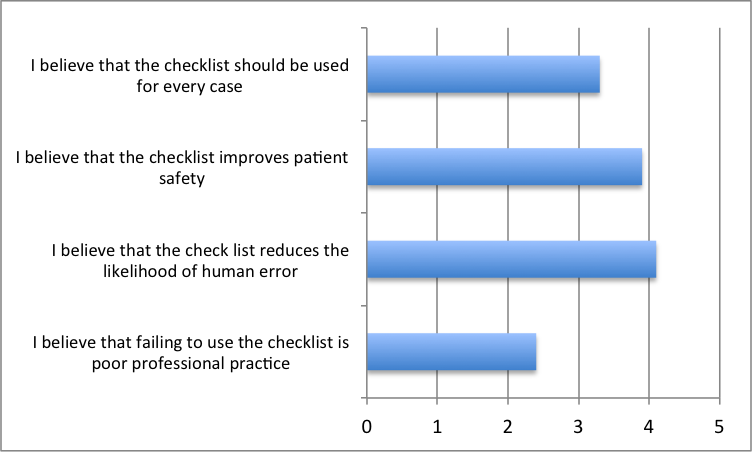
We asked people to rank the following statements from 1-5, with 1 being strongly disagree and 5 being strongly agree. The average score is shown on the chart below.
Comments about the checklist.
"Ensures everyone is aware of plans for the RSI, staff are less likely to panic if a problem dose arise, members of the emergency departmement (not just left to the ODP and anaesthetist) are aware and can assist with cricoid/ drugs"
"Stops me forgetting something essential in the times when you might be stressed/ rushed"
"Easy to use, good reminder"
"Can not always get all team members to engage with checklist. Resistance from ODP's who see it as a challenge to their professional practice"
"Used them before I think it improves safety and allows you to function at a higher level. not having to remember equipment frees your mind to concentrate on the medicine"
 Send Email
Send Email