


Theme
8JJ Patient safety
INSTITUTION
Royal Free Hospital NHS Trust
Every year nearly 2000 people get meningitis or meningococcal septicaemia in the UK, majority of them children. Currently, 1 in 10 children affected will die or have a life time cost of 6 million US$, if seriously disabled by it. The British Medical Journal identified high mortality rates when trainee doctors were unsupervised while reviewing patients with potential septicaemia or meningitis1
Out of the 60 trainees:
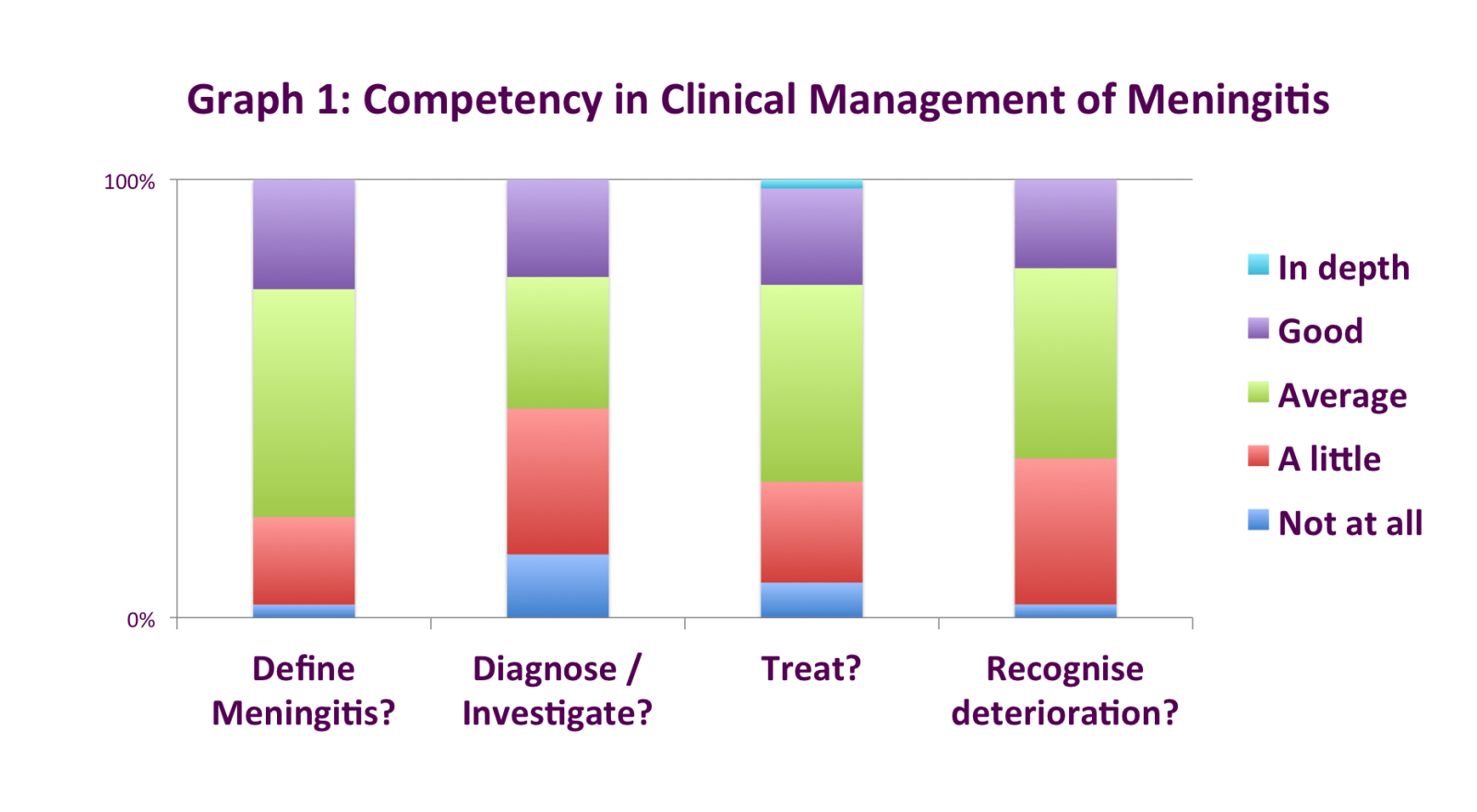
- 1 in 3 felt they had 'very little' competency in diagnosing, investigating, treating and recognizing a deteriorating child, illustrated in Graph 1
- Half of the trainees were unaware of the local protocol
- 7 in 10 had no real life simulation exposure to cases in their training.
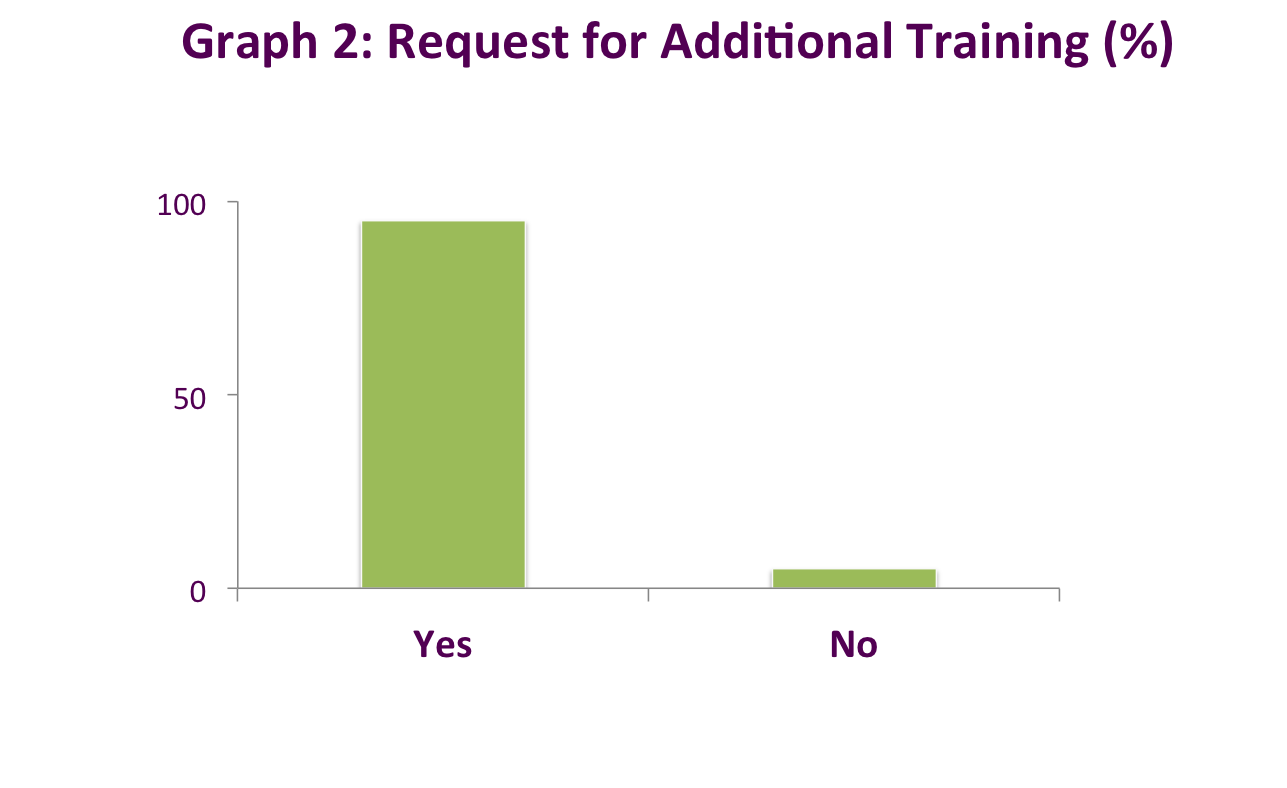
- 95% felt additional teaching would be beneficial (Graph 2)
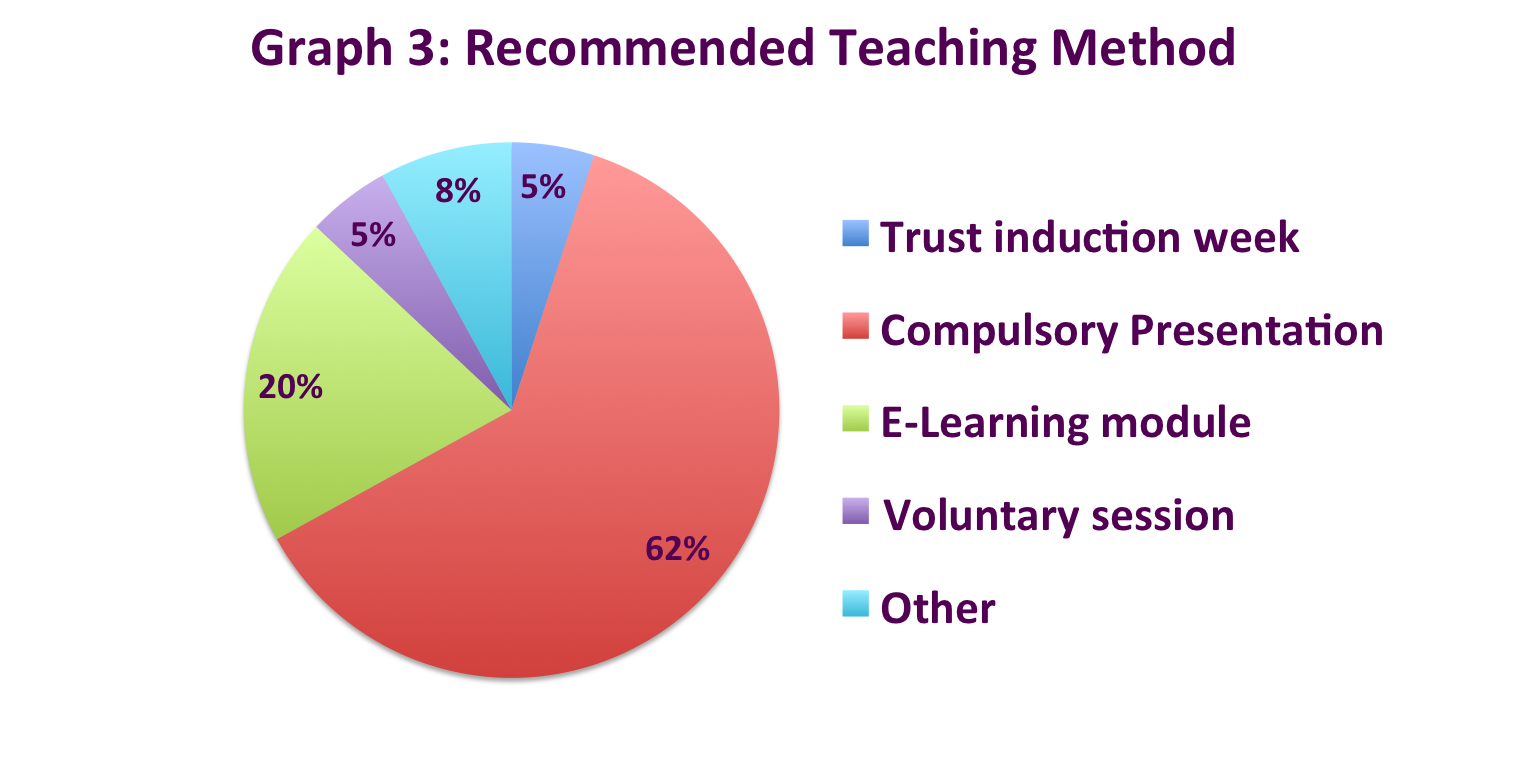
- 62% recommended a compulsory presentation (Graph 3)
Suggestions included:
- ‘examples by clinical cases’
- ‘early teaching for paediatric trainees in particular’
- ‘easy to access’ resources
An online tool was created to understand preparedness of Foundation Year 1 and 2 doctors at the Royal Free Teaching Hospital, London.
- 7 questions related to competency on the management pathway of Meningitis
- 3 questions were centered on education and training.
- Questionnaire available on request
Watch our brief video on responses from doctors in our study and our follow-up intervention (link or QR scan):
https://www.youtube.com/watch?v=_igxY2C1Jqs

There is a lack of confidence amongst Junior Doctors in competency for managing meningitis.
This gives an opportunity to enhance patient safety and reduce mortality by improving further education and awareness of such a common, severe condition.
This can be done using a range of resources to improve training including wide-access electronic medium and simulation in the curriculum.
What next?
Two resources were put in place to increase learning opportunities:
- An interactive slide-show, for group or self learning, was created based on the handbook by Meningitis Research Foundation’s ‘Lessons from research for doctors in training’, using real cases with unwanted outcomes as learning tools2.
- Posters around the hospital highlighting trust guidelines.
A follow-up study is currently being done to explore the usefulness of posters as a tool for education around clinical areas - click on ‘more details‘ for latest results.
1. Ninis et al. The role of healthcare delivery in the outcome of meningococcal disease in children: case-control study of fatal and non-fatal cases , The British Medical Journal 2005; 330:1475, doi: http://dx.doi.org/10.1136/bmj.330.7506.1475
2. Nini N, Nadel S, Glennie L. Lessons from research or doctors in training: Recognition and early management of meningococcal disease in children and young people. 3A ed. Bristol: Meningitis Research Foundation; 2013. http://www.meningitis.org/assets/x/50156 [Accessed 15 March 2014]
With thanks to:
Royal Free Hospital NHS Trust, Paediatric Department
UCL Partners


 Send Email
Send Email