
| Theme: 4JJ Interprofessional education 1 | |||
 |
||||||
| Nursing faculty teaching nursing skills to medical students: a Lebanese experience |
 |
|||||
|
||||||
Background
- Nursing faculty teaching medical students basic nursing skills is a relatively new trend.
- Collaboration in education among medical and nursing professions can improve students’ performance in clinical skills and consequently positively impacts the quality of care delivery.
Summary of Work
- In 2011, the Faculty of Medicine at the University of Balamand, Lebanon, launched a "nursing skills" module as part of clinical skills teaching to MED-1 students.
- The module is prepared and delivered by nursing faculty in a laboratory setting. It consists of informative teaching as well as hands-on laboratory practice.
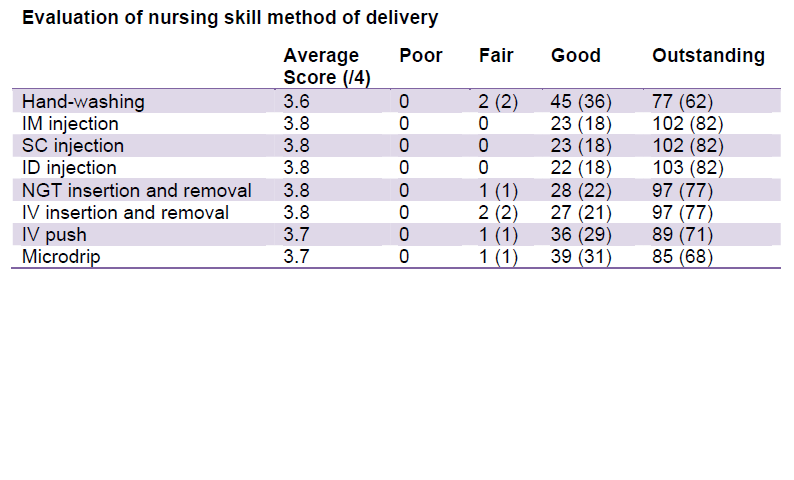
- The skills taught are:
- hand-washing
- medication administration
- intravenous initiation and removal
- nasogastric tube insertion and removal
- Sixty-five medical students attend this module every year.
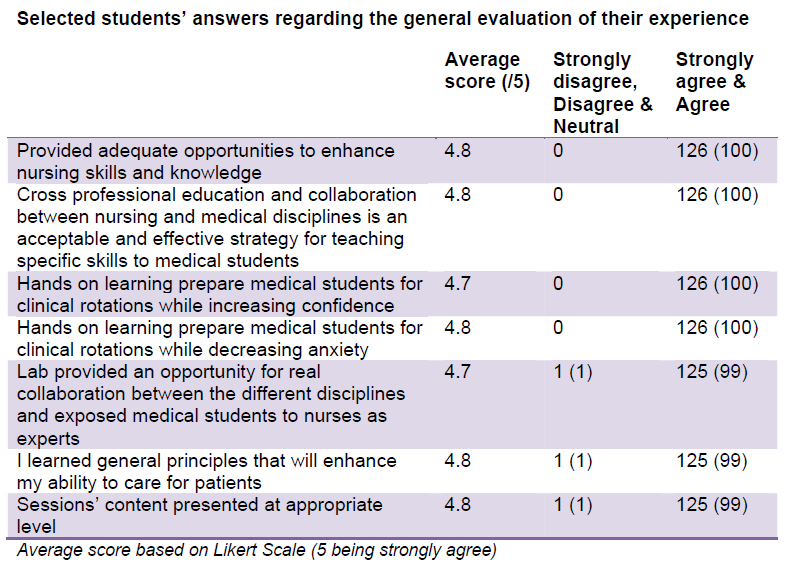
- A Likert-scale-based questionnaire is used to evaluate their experience.



Acknowledgement
- Nadim Karam, MD, MPH - Dean of the Faculty of Health Sciences at the University of Balamand
- Camille Nassar, PhD - Dean of the Faculty of Medicine and Medical Sciences at the University of Balamand
Summary of Results
- Medical students agree that the module provides adequate opportunities to enhance nursing skills and knowledge and favor cross-professional education between nursing and medical disciplines.
- Most of the respondents report that this experience prepares them better for clinical rotations while increasing their confidence and decreasing anxiety level.
- Medical students highly appreciate the nursing faculties’ expertise and perceive them as knowledgeable and resourceful.
Conclusion
Nursing faculty participating in medical students skills teaching is well perceived, has a positive impact and shows nurses as proficient teachers to medical students.
Take-home Messages
Cross-professional education is an attractive model when it comes to teaching nursing skills in medical school.
References
- Barr, H. (1996). Interprofessional Education in the United Kingdom. Some Historical Perspectives 1966-1996. Retrieved from www.caipe.org.uk/silo/files/cipw-historical-perspectives.pdf
- Bradley, P., Bond, V., & Bradley, P. (2006). A questionnaire survey of students’ perceptions of nurse tutor teaching in a clinical skills learning program. Medical Teacher, 28 (1), 49-52.
- Elms, S.A. & Chumley, H. (2006). Nursing faculty teaching basic skills to medical students. Medical teacher, 28 (4), 341-344.
- Tucker, k., Wakefield, A., Boggis ,C., Lawson, M., Roberts, T., & Gooch, J. (2003). Learning together: clinical skills teaching for medical and nursing students. Medical Education, 37, 630-637.

 Send Email
Send Email