


Theme
2JJ Communication
INSTITUTION
University of St Andrews - Medical School

Communication training and assessments can provoke anxiety in medical undergraduates, including when working with simulated patients, or with video feedback[1-3]. A quarter of students experiencing academic difficulties express problems approaching patients[4]. Our recent work showed that medical students were reticent to take part in workshops focussed on providing coping skills for communication-related anxiety due to stigma associated with admitting to experiencing anxiety[5].
There is evidence that medical students often replace positive coping strategies, like seeking professional help, with less useful long-term strategies like increased alcohol consumption[6]. Despite experiencing high levels of mental wellbeing issues, doctors are also less likely to seek help in comparison to other working populations[7]. Reducing the stigma associated with mental well-being issues, including communication-related anxiety, in the early stages of a student’s training may have important long-term effects for help-seeking after qualification. However, if we are to do this we need a greater understanding of the current experiences and views of students towards communication-related anxiety and admitting to mental wellbeing issues to others, such as peers and staff. The aim of this study was to identify factors influencing medical undergraduate experiences of communication-related anxiety and their support seeking behaviour for such difficulties.
An online questionnaire was circulated to medical students across participating UK Medical Schools (n = 15) which included scales measuring social interaction anxiety[8], perceived stress [9], attitudes towards communication training[10], support seeking behaviour and alcohol use [11]. Participants were recruited by e-mail or VLE announcements and used the link provided within the advert to access the information and consent form. Once the consent form was completed, participants could access the survey. This study was approved by the University of St Andrews Teaching and Research Ethics Committee and ratified by individual Medical School ethics boards where appropriate.
Sample
Table 1: Demographic characteristics of consenting participants
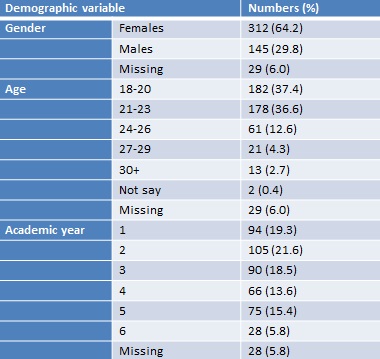
A total of 486 participants completed the questionnaire, from 15 UK Medical Schools, demographic information of this sample is shown in table 1.
Impact of gender on experience of anxiety
Figure 1: Gender differences in how participants score on each scale. SIAS = Social Interaction Anxiety Scale, PSS = Perceived Stress Scale, CSAS = Communication-Skills Attitudes Scale, AUDIT-C = drinking practices.
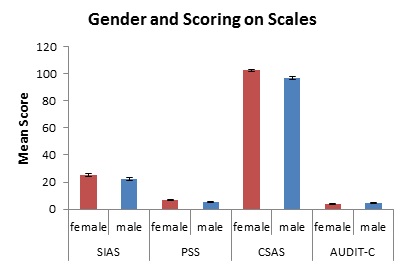
Gender played a key role in the experience of social interaction anxiety (SIAS: Female mean = 25.3, Male = 22.2, t = 2.2, df = 281.4, P = 0.035), perceived stress (PSS: F = 6.89, M = 5.39, t = 3.93, df = 416, P = 0.0001), attitudes towards communication training (CSAS: F = 102.4, M = 96.87, t = 3.86, df = 430, P = 0.0001) and alcohol consumption (AUDIT-C: F = 3.71, M = 4.79, t = -3.92, df = 384, P = 0.0001).
Figure 2: Gender differences in the nervousness experienced with interactions that are common-place during communication-skills training. Scale based on likert where 0 = “not at all” and 4 = “extremely”.
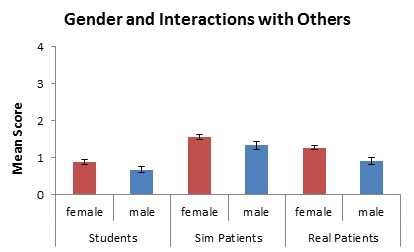
Female participants reported being significantly more nervous when speaking with real patients (X2= 12.669, df = 4, P = .013). Although there was a trend for female participants to report being more nervous when speaking with fellow students (X2 = 5.488, df = 4, P = .241) and simulated patients (X2 = 4.197, df = 4, P = .380), these differences did not reach statistical significance.
Impact of gender on help seeking attitudes and behaviour
Figure 3: Histograms generated from individual scale items. The pattern of scoring shows two peaks at “disagree” and “agree”.
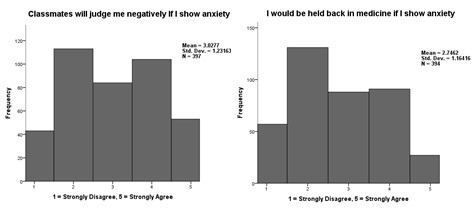
Participants give dichotomous responses regarding whether they agreed or disagreed that peers and medicine in general would view them negatively if they admitted anxiety – Figure 3, possibly reflecting two different views held by medical students. There were no gender differences in the responses to these questions.
Figure 4: Histograms showing distribution of scoring on items relating to where students seek support.
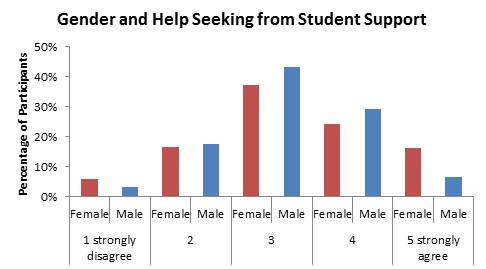
When examined by gender, females are less likely agree that it was easy to talk with Student Support Services about personal difficulties – see Figure 4; however, this difference does not quite achieve significance (X2 = 8.291, df = 4, P = .081).
Figure 5: Histograms showing distribution of scoring on items relating to where students seek support.
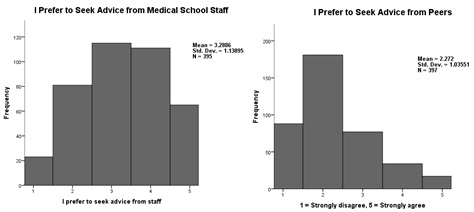
There are no gender differences regarding whether participants would seek help from peers or medical school staff regarding difficulties with coursework.
Gender and other factors influenced participant experiences of communication-related anxiety and support seeking. This greater understanding of student experiences of and their attitudes towards communication-related anxiety and stress will assist in developing acceptable support.
Medical Schools should aim to create an environment whereby all students are confident in seeking support for communication-related anxiety.
Thanks to the Medical School, University of St Andrews for supporting this study.
1. van Dulmen S, Tromp F, Grosfeld F, ten Cate O, Bensing J: The impact of assessing simulated bad news consultations on medical students' stress response and communication performance. Psychoneuroendocrinology 2007, 32:943 - 950.
2. Humphris G, Laidlaw A: The use of Reflection-on-Action in medical undergraduate communication skills teaching with naïve and experienced students. EACH 2006.
3. Lindon-Morris E, Laidlaw A: Anxiety and selfawareness in video feedback. The Clinical Teacher 2014, 11:174 - 178.
4. Sayer M, Saintonge MCD, Evans D, Wood D: Support for students with academic difficulties. Medical Education 2002, 36:643 - 650.
5. Dennis A, Warren R, Neville F, Laidlaw A, Ozakinci G: Anxiety about anxiety in medical undergraduates. The Clinical Teacher 2012, 9:330 -333.
6. Ball S, Bax A: Self-care in medical education: Effectiveness of health-habits intervention for first-year medical students. Academic Medicine 2002, 77(9):911 - 917.
7. Holmes J: Mental Health of Doctors. Advances in Psychiatric Treatment 1997, 3:251 - 253.
8. Mattick R, Clarke J: Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behavior Research and Therapy 1998, 36:455 - 470.
9. Cohen S, Kamarck T, Mermelstein R: A global measure of perceived stress. Journal of Health and Social Behaviour 1983, 24:385 - 396.
10. Rees C, Sheard C, McPherson A: Communication skills assessment: the perceptions of medical students at the University of Nottingham. Medical Education 2002, 36:868 - 878.
11. Bush K, Kivlahan D, McDonell M, Fihn S, Bradley K: The AUDIT Alcohol Consumption Questions (AUDIT-C): An Effective Brief Screening Test for Problem Drinking. Archives of Internal Medicine 1998, 158:1789 - 1795.
 Send Email
Send Email